Provider Incentive Payment Solution
Simplifying the administration of value-based payments.
Provider Incentive Payment Solution
Are you ready to reward your providers for delivering high-quality and cost-efficient care?
Is it time to move to paying providers based on value instead of fee-for-service?
Valiant Health has created a Provider Incentive Payment Solution (PIPS) that gives you the freedom to customize reimbursement models that will incent behavior and help manage contracts.
Valiant Health’s PIPS allows you to share a dashboard with your providers, so they can self-report their quality results quickly and efficiently back to the payer.
Additionally, our solution also allows you to create bonus programs and campaigns to offer to individual providers or to your own care management team.
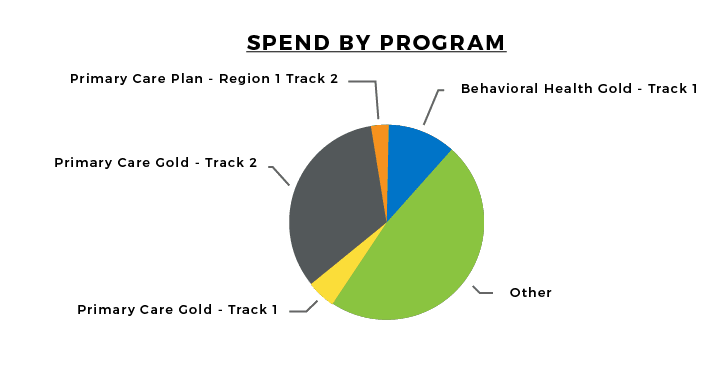
Through all the data that we gather with our solution, we are able to provide flexible reporting to streamline both provider financial payments and internal analyses.
PIPS also enables comparative analyses so you can compare provider versus provider, region versus region, and much more.
Analytics & Reporting: Programmatic Action
• Provider Scorecards
• Flexible Drill-Down Reporting
• Efficient Analytics
• Comparative Analyses
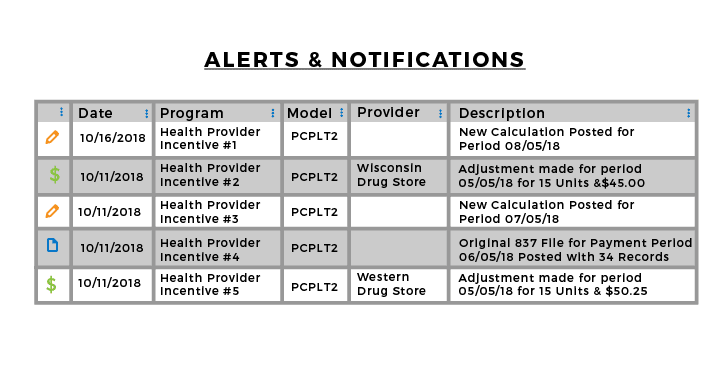
Notifications for key activities such as new payments, approvals, and adjustments are visible and can be searched within the application along with a current work queue so tasks get finished.
Dashboard View:
Easy Reference
• Save Time through Workflow Simplification
• Manage Provider Contracts